Endodontic (Root Canal) Treatment
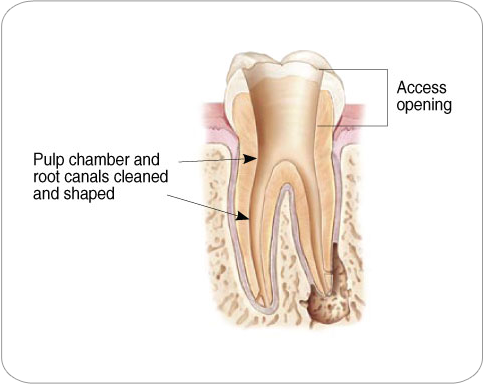
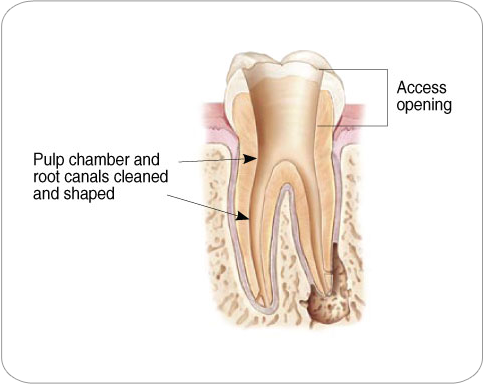
Endodontic treatment can often be performed in one or two visits and involves the following steps:
Frequently Asked Questions about Endodontic Procedure
What does the term Endodontic (Root Canal) Treatment mean?
To understand endodontic (root canal) treatment, it helps to know something about the anatomy of the tooth. Inside the tooth, under the white enamel and a bone-like layer called the dentin, is a soft tissue called the pulp. The pulp contains blood vessels, nerves, and connective tissue and helps to form the crown of the tooth and to grow the root(s) during development.
The pulp extends from the crown of the tooth to the tip of the root(s) where it connects to the ligament and bone tissues surrounding the root. The pulp is important during the growth and development of the tooth. However, once a tooth is fully mature it can survive without the pulp, because the tooth continues to be nourished by the ligament and bone tissues surrounding it.
Why would I need an Endodontic (Root Canal) procedure?
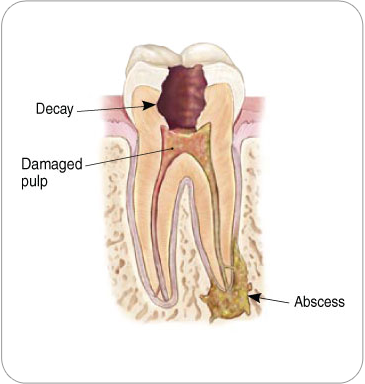
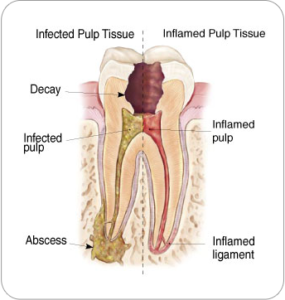 Endodontic (Root Canal) treatment is necessary when the pulp, the soft tissue inside the root canal, becomes inflamed or infected. The inflammation or infection can have a variety of causes: deep decay, repeated dental procedures on the tooth, or a crack or chip in the tooth. In addition, an injury to a tooth may cause pulp damage even if the tooth has no visible chips or cracks. These variety of causes allow the microorganisms to enter the pulp and set off the inflammation in the root canal space. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess may cause swelling.
Endodontic (Root Canal) treatment is necessary when the pulp, the soft tissue inside the root canal, becomes inflamed or infected. The inflammation or infection can have a variety of causes: deep decay, repeated dental procedures on the tooth, or a crack or chip in the tooth. In addition, an injury to a tooth may cause pulp damage even if the tooth has no visible chips or cracks. These variety of causes allow the microorganisms to enter the pulp and set off the inflammation in the root canal space. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess may cause swelling.What are the signs of needing Endodontic (Root Canal) treatment?
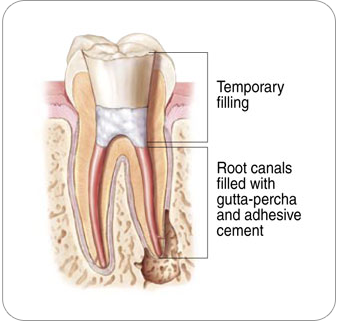
How does Endodontic (Root Canal) Treatment save the tooth?
Will I feel pain during or after the Endodontic (Root Canal) procedure?
Endodontist (Root Canal Specialists) are experts in managing pain caused by inflamed or infected pulp. Ask endodontist (root canal specialists) about how best to manage pain before the endodontic (root canal) procedure begins.
For the first few days after treatment, your tooth may feel sensitive, especially if there was pain or infection before the procedure. This discomfort can be relieved with over-the-counter or prescription medications such as ibuprofen and acetaminophen. If necessary, the endodontist (root canal specialist) will prescribe pain medications to keep you comfortable.
Your tooth may continue to feel slightly different from your other teeth for some time after your endodontic (root canal) treatment is completed. However, if severe pain or pressure or pain that lasts more than a few days, call the endodontist (root canal specialist).
How much will the Endodontic (Root Canal) Treatment cost?
Generally, endodontic (root canal) treatment and restoration of the natural tooth are less expensive than the alternative of having the tooth extracted. An extracted tooth must be replaced with a bridge or implant to restore chewing function and prevent adjacent teeth from shifting which can cause discrepancy in biting. The procedures to replace the extracted tooth with a bridge or dental implant tend to cost more than endodontic (root canal) treatment and the follow up restoration. Root canal treatment not only saves natural teeth and but also money.
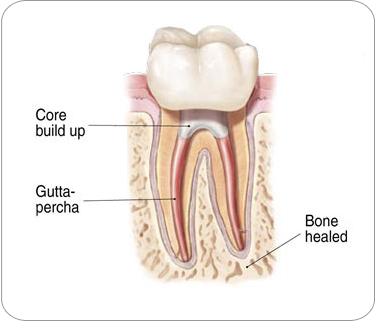
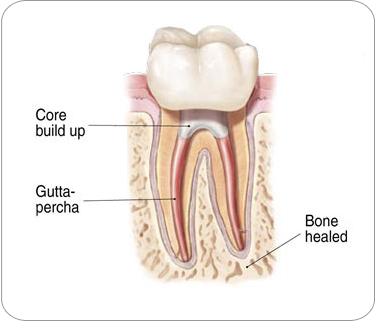
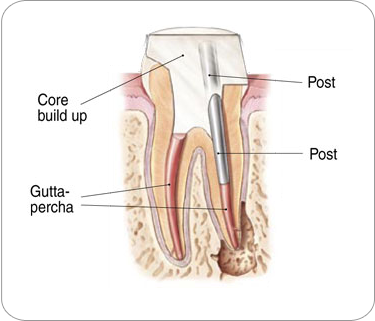
Will the tooth need any special care or additional treatment after Endodontic (Root Canal) treatment?
Most endodontically treated teeth last as long as other natural teeth. In a few cases, a tooth that has undergone endodontic (root canal) treatment does not heal or the pain continues. Occasionally, the tooth may become painful or diseased months or even years after successful treatment. Often when this occurs, revising the endodontic (root canal) procedure or surgical procedure can save the tooth.